How an Ohio Middle Suburb Is Tackling Its Opioid Epidemic

Last year, Lake County, a Middle Suburb just east of Cleveland, Ohio, set a grim record. In 2017, overdose deaths were at the highest levels ever reported in the county, echoing a trend seen across the state, and the country.
Lake County leaders know that opioid addiction is a chronic disease requiring public health action from multiple angles. “Drug abuse is multifaceted,” says Matthew Nichols, Lake County Health District planning, research, and policy coordinator II. “It’s not something that is going to be a one-pronged fix.”
The health district’s dedicated team is working both on the front lines and in the back room to develop proactive solutions. “Much of public health [work] when it comes to opiate addiction is based off of overdose deaths,” Nichols says. “And for us, that’s too little too late.”
Lake’s Growing Problem
Lake County is a blue-collar community where nearly one-fifth of employment comes from manufacturing. Lake’s roughly 230,000 residents are primarily white (92%) and have a median household income of $59,958, above the national median of $55,322. The county scores well on many health indicators — uninsured rates (7%), for example, are below the national average (11%).
But Middle Suburbs like Lake County have been hit particularly hard by the opioid epidemic. This community type’s median drug overdose rate, 26 overdoses per 100,000 people, is the highest of any type in the ACP. Lake County’s rate is even more dire: 31 overdoses per 100,000 people.
Over the last five years, opioid cases have nearly tripled in Lake County, from 296 cases in the crime lab in 2013 to 868 cases in 2017. Like other parts of the country, Lake has seen a drastic increase in fentanyl and fentanyl analogs.
Revealing Who is At Risk

Community leaders have rushed to respond to the growing epidemic in every way possible. “We are going into surgery with a chainsaw most times,” says Ron Graham, the Lake County Health District’s commissioner.
By identifying people and places most at risk, Lake County hopes to take a more targeted approach. The health district recently released a report analyzing overdoses from 2013 to 2017. This type of detail allows them to “go into surgery with a scalpel,” Graham says.
The report found that most Lake County residents who died from an overdose were male (72%) and Caucasian (98%). It also revealed three other common factors in overdoses: most occurred at home, the majority of individuals were working age (25 to 54 years old) and nearly half held labor, trade or manufacturing occupations.
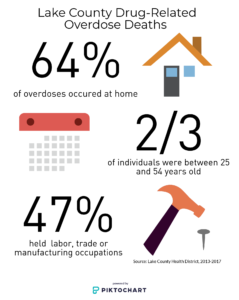
“In order to combat a problem, you have to know what that problem is,” says Nichols. Because 47% of fatal overdoses involved individuals with labor, trade or manufacturing occupations, the health district wants to team up with employers in those industries. “There has been some occupational-specific programming in the past, but I really think that’s something we will look at much more closely now,” Nichols says.
For example, the health district is exploring a program called Screening, Brief Intervention, and Referral to Treatment, or SBIRT, which could quickly identify employees suffering from addiction and connect them with help. Graham is also assisting Lake’s Alcohol, Drug Addiction, and Mental Health Services (ADAMHS) Board in designing programs for high school students going directly into the workforce after graduation.
Listen to Nichols and Graham discuss what their report revealed about occupation and overdoses, and how they plan to partner with local businesses.
Fighting Addiction From All Angles
Lake County initiatives also include a prescription drug monitoring program, overdose education and drug treatment efforts, among others.

One effort already showing success is Project DAWN (Deaths Avoided with Naloxone), a state-wide overdose education and naloxone distribution program. Through this project, the Lake County Health District has given out more than 350 free kits containing the overdose reversal medication. About 60% of people reported they obtained the naloxone kit for their child or another family member, explains Planning, Research, and Policy Coordinator Jessica Wakelee. “Very few were going to be personally used,” she says. Of the 19 people who came back for a new kit, 17 had successfully reversed an overdose, one outcome was unreported, and one was a fatality.
“You see many different faces come through the door,” Lake County Health District Health Educator Haley Russo said of Project DAWN in an email. “I have heard many stories, mostly from mothers and grandmothers of the addicts and I know all I can do is listen. They are scared, desperate and are willing to do anything to save their child or grandchild from a potential overdose death.”

Lake County is also working to map opioid addiction by way of a framework called agent-based modeling. Though agent-based modeling has been widely used in other fields, the health district would be among the first to apply this modeling approach to opioid abuse at a county level.
Using a predefined model pathway based on a number of demographic variables, agent-based modeling will help the county to quantify approximately how widespread its opioid problem is, and which residents may be most at risk for opioid abuse. This information will allow the county to be more proactive in programming, such as identifying high-priority naloxone distribution areas.
Listen to Matt Nichols explain how agent-based modeling can help the county expand its view of the opioid epidemic.
Read more about Lake County’s overall health in the American Communities Project’s new report “Health and Place in America, 2018.”
